Bioprinting has transitioned from an ambitious idea to a field making steady progress toward creating functional tissues and vascularized structures, offering a glimpse into the future of regenerative medicine.Against this backdrop, Professor Mark Skylar-Scott shared his insights into the current state and future of bioprinting in an exclusive interview with 3DPrint.com.Despite remarkable progress in recent years, bioprinting remains a field where the potential often clashes with challenges.
Creating functional, vascularized tissues that can thrive in clinical environments is still a major hurdle.Skylar-Scott co-created SWIFT at the Wyss Institute, one of the earliest platforms designed to simplify and speed up vascularized tissue fabrication, and now leads cutting-edge research at Stanford University to tackle these obstacles head-on.“Bioprinting is still in a position where it needs to prove itself,” Skylar-Scott stated.
“Despite the rapid advances in hardware, materials, and accessibility, there is still no bioprinted product on the market.Even “simpler” non-bioprinted tissue-engineered products are rare.In fact, the ultimate challenge lies in function—creating bioprinted structures that truly replicate the strength, flexibility, and functionality of natural tissues.” Mark Skylar-Scott.
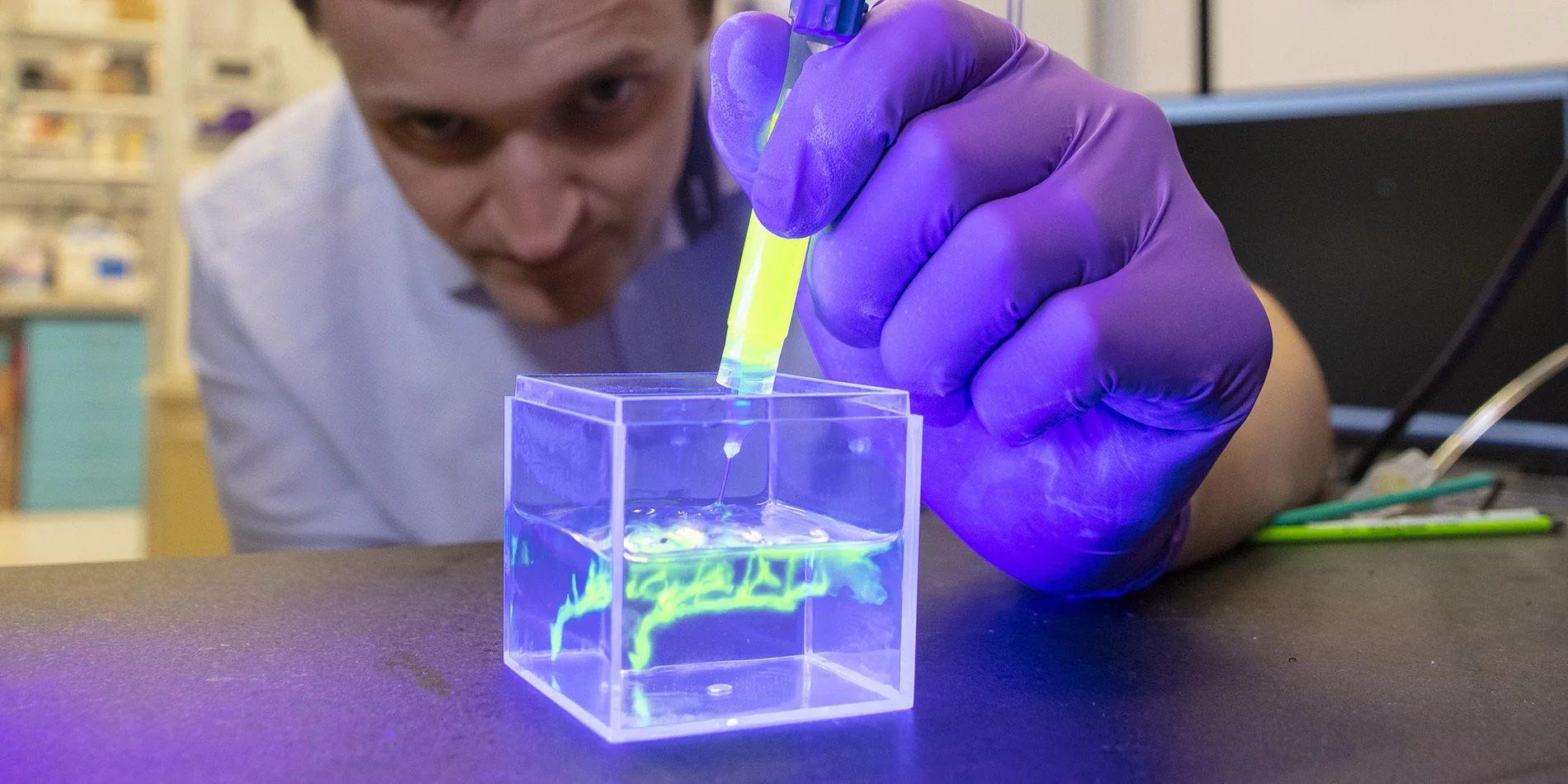
Image courtesy of Stanford University.What’s more, Skylar-Scott highlights the gap between aspiration and reality, asking: “Can we print a bone that’s as strong and complex as a living bone? No.Can we print a ligament that’s as strong and complex as a living ligament? No.
Can we make a fully 3D printed heart yet? Not yet.” His observations point to a need for breakthroughs in vascularization and organ-scale printing.One of the most critical issues in bioprinting is vascularization, the ability to create blood vessel networks that nourish and sustain large, complex tissues.The expert says that the bioprinting community can print big vessels and even some small ones, but there is no example yet of a vascular tree that spans from large vessels to capillaries.
This problem, once thought to be solvable through self-assembling small vessels, has proven much harder than expected.However, he is optimistic about recent developments in biology and materials science.Recent results from Professor Milica Radisic’s laboratory at the University of Toronto show that adding primitive macrophages can dramatically improve the microvascularization of cardiac tissues.
A second promising approach, known as sacrificial molding, has recently been piloted by numerous laboratories.It involves incorporating noodle-shaped microfilaments—thin, temporary structures—into tissue scaffolds.These microfilaments act as placeholders for vascular networks or fluid channels.
Once the scaffold is formed, the microfilaments are removed by dissolving or melting them away, leaving behind intricate, interconnected networks of hollow channels.This sacrificial method shows significant potential for creating the multi-scale vascular systems required to sustain large, complex tissues.“I think we’ll start to see the first convincing papers showing scalable vascularization within the next one to two years.
These studies will demonstrate how we can create vascular trees that span many orders of magnitude length scales and create perfusable channels, which is a critical step for the field.” When asked about the timeline for transplantable or clinically trialed organs, Skylar-Scott stressed the long and arduous road ahead: “If we’re talking about fully bioprinted organs routinely used in humans, we’re likely looking at 20 to 30 years.However, the field could see its first clinical trials for specific constructs, such as bioprinted pancreatic tissue or vascularized beta islet cells for diabetes, within a decade.” A 3D bioprinter in the Skylar-Scott lab prints a sample of heart tissue in 2022.Image courtesy of Andrew Brodhead/Stanford University.
“The momentum right now is in smaller, more achievable constructs.For instance, numerous companies have recently been funded for bioprinting beta islet cells that could potentially revolutionize diabetes treatment,” he explained.Skylar-Scott explained that smaller constructs, such as a vascularized centimeter cube of beta islet cells for diabetes, represent a pragmatic first step for 3D bioprinting and are more readily achievable than fully functional organs.
These steps not only address critical challenges like scalable vascularization and efficient cell production but also provide proof of concept, helping to demonstrate tangible progress and attract more investment.Focusing on small steps helps researchers tackle the challenges of creating entire organs.Another critical area of focus for 2025 is speeding up bioprinting processes.
Skylar-Scott pointed to advances in volumetric 3D printing and parallelized printing systems, which aspire to overcome the “cubic law” that causes print times to spiral out of control with increasing tissue size.According to this principle, printing larger tissues takes much more time because a tissue’s volume grows much faster than its length.Traditional layer-by-layer printing can’t keep up, as bigger constructs need far more material and take much longer to print.
New technologies like volumetric printing and parallelized extrusion systems tackle this problem by printing multiple layers or entire volumes at once, making it quicker and more efficient to create large tissues.“High-throughput printing will be essential to scaling up organ production,” he said.Equally important is the challenge of cell production: “If you want to make something big, you need a lot of cells.
For instance, a bioprinted heart requires roughly 30 billion cells.Our lab at Stanford is scaling up production to 10-liter bioreactors, capable of producing enough cells for organ-scale experiments.Still, the costs, both in terms of labor and materials, are a substantial barrier.
We’re working hard to make cell production more sustainable and efficient, but it’s still incredibly expensive.Reducing these costs is crucial to ensuring that bioprinting remains viable for widespread clinical use.” Skylar-Scott believes that public perception remains a challenge.He says bioprinting was swept up in the 3D printing hype cycle about ten years ago, and it is now successfully crawling out of the valley of disappointment and into a more realistic, exciting, and pragmatic phase.
He believes that showing tangible and functional results—like a kilogram of vascularized, beating human tissue—will capture public and scientific attention, reigniting enthusiasm for the field.As bioprinting moves closer to clinical applications, interdisciplinary collaboration will be key, which is why Skylar-Scott’s lab integrates biologists, engineers, and surgeons to tackle the field’s most pressing challenges.One example is their major goal of recreating a human heart for implantation into a pig with mutations to prevent human tissue rejection.
Skylar-Scott’s message was clear: bioprinting is making strides, but there are no shortcuts to success.“We will continue to prioritize function in our publications.Credibility is key in a field that has been plagued by hype.
Our goals are certainly lofty, but we are truly taking the bold steps that we think are necessary to move us forward.” Looking ahead, Skylar-Scott’s lab’s ambitious goals represent the forefront of bioprinting innovation, from achieving scalable vascularization to producing organ-scale tissues.While routine use of bioprinted organs may be decades away, 2025 promises to be a key year for laying the groundwork.“We’re on the upswing, moving beyond talk and into tangible progress.
It’s an exciting time to be part of this field, and I consider myself lucky to be working with so many talented and dedicated students and scientists” concluded Skylar-Scott.Subscribe to Our Email Newsletter
Stay up-to-date on all the latest news from the 3D printing industry and receive information and offers from third party vendors.